NHS England Inequalities Resource on Access to Primary Care
Here’s the problem. Health Inequalities continue to grow (Kings Fund 2017) and many people who under the Equalities Act are described as having “protected characteristics” such as people with disabilities and mental health problems have seen little improvement in their circumstances (Being Disabled in Britain April 2017).
So, I was pleased to see the launch of the NHS England Inequalities Resource for reducing inequalities in access to general practice.
I have spent the last 4 years or so working with GP, Public Health and Voluntary sector colleagues trying to develop a stronger focus on health inequalities in primary care, problems include:
-
The challenges faced by GPs working in very disadvantaged communities are insufficiently understood and more importantly insufficiently owned at a local health system level.
-
Much guidance fails to sufficiently recognise the social and economic circumstances that affect people’s health and their ability to take control.
-
Many GPs who don’t serve communities who experience multiple disadvantage struggle to understand the complexity of the challenge and why their peers need additional resources.
In many places there are GPs who have dedicated their working career to responding to the needs of disadvantaged groups – such as the homeless, substance misusers and people with a learning disability. Many of them work in economically deprived neighbourhoods – these often have higher numbers of people with protected characteristics too.
Does this resource help?
Well, it is good that it has been produced – better something than nothing in my view – it gives us something to build on.
It is clear that a small team of people have worked hard to pull together existing knowledge into one place. Regrettably the layout is not up to the task of making this information accessible – its largely a gateway to further large and complex documents rather than an expert analysis of this complex issue.
This document says it is for CCGs and GPs. I don’t think it is. It offers little challenge to CCGs and no coherent view about what actions CCGs should take to tackle inequalities. I think the main audience are trainee GPs and other relatively new staff working in primary care settings – there is nothing wrong with this but it does not do what it says on the tin.
Its not the fault of the authors of the document but its existence highlights where the deficits are:
- Tackling inequality is NOT an issue that is experienced in the same way across local health systems. For GPs serving very deprived communities this is the day job – for others inequality is not a systemic issue. This disparity creates an unbalanced discourse at a local level.
- in my view experienced GPs and their collaborators need help developing strategies to change the hearts and minds of their peers and CCG officers who are not working in disadvantaged communities and that will help challenge CCGs and Accountable Care Systems to raise their game and their priorities.
We need to recognise that this issue exists primarily because of an imbalance in power – not because of a lack of skills and knowledge. It is a truism that services that seek to respond to the needs of people who lack power are themselves disempowered.
What we need next
We need to establish a systematic and ongoing programme of knowledge exchange – we can learn from the models of the last Labour Government – see David Bucks Kings Fund blog here and most importantly check out Reducing Health Inequalities – System, Scale and Sustainability from Public Health England who have asked the Chris Bentley to share the learning from the Labour Government’s National Support Team for Health Inequality.
NHS England and Public Health England needs to commission a long term system change programme here. Its not just for General Practice to do the changing – that will be easier if we get the right leadership at a local level.
It would help to have:
- Strategic Analysis of the local equality/health inequality challenge its scale and why it exists – at a place level.
- Advocacy at a national level for explicit local strategies to tackle inequality
- Clear examples of systemic models that can be used to create change
What do you think?
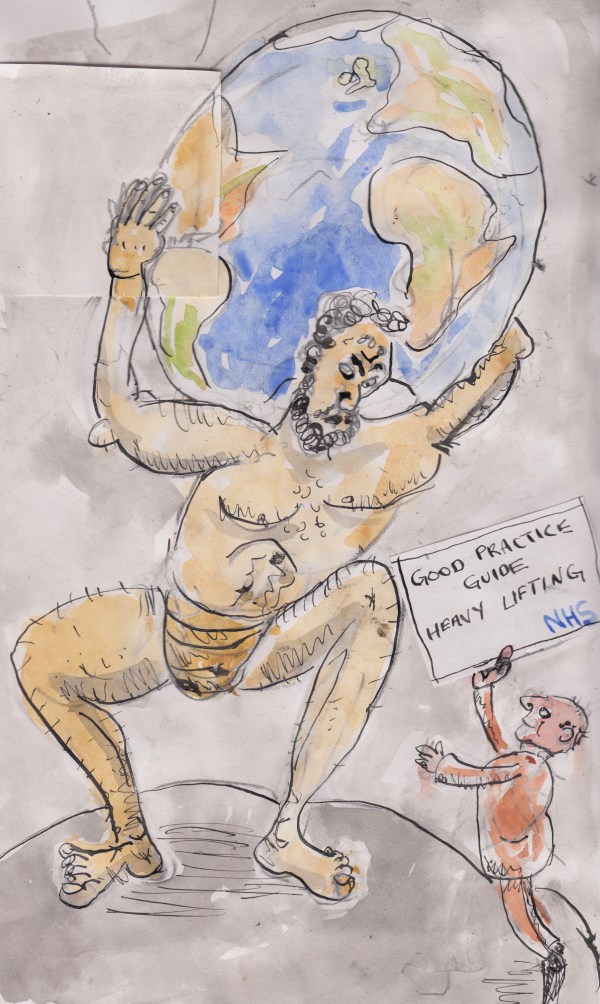
Good luck with this heavy lifting Mark. A better knowledge exchange might help a bit but what we really need is regime change!
Cheers Mike – agree completely – however, even during the labour government period there was insufficient recognition of the challenges faced by GPs serving communities experiencing disadvantage. As I say in the blog it feels as though GPs serving these communities are in effect ghettoised working to a different analysis of what inequalities means and what its causes are compared to their peers in better off areas. Part of the challenge is changing the perspective of the wider body of the medical profession who do not ‘feel’ the issues experienced by the bottom 20% of the population on a daily basis.
Mark you have “hit the nail on the head” so to speak. Having worked as a GP in several “deprived communities” over past years I always I found myself too busy in such GP practices to have time to attend meetings and make the case for more / different or better resources. Now that we have CCGs we also need colleagues within each CCG to identify areas and practices that need extra support/ identify the kind of support needed and use political skills to obtain the resources and support needed. One size does not fit all. .
Thanks Malcolm – agree completely – we need a clear institutional analysis – which I think we lack at the moment and as you say this analysis will vary from place to place to some degree
At a GP conference in the South West of England a few years ago I found myself talking with several GPs undertaking “vocational training” of a different kind . They were studying GP work half time and Public Health part time. All were enjoying the Public Health sessions but felt very frustrated that their next step as medics would have to be into Full Time GP work because at that time no CCG was offering GPs sessions in Public Health. Maybe things have changed but it occurs to me that we should be trying to find the GPs who have experienced an introduction to Public Health thinking and practice to undertake the much needed “institutional analysis” which we currently lack.
Thanks Mark – well said.
You might have told me about this paper (apologies if so!) but this is useful:
Browne et al. International Journal for Equity in Health 2012, 11:59
http://www.equityhealthj.com/content/11/1/59