Rare Cancer? You’re on your own kid!
This blog is about how people with rare cancers seem to be left on their own by the NHS and leading cancer charities it is based on my personal experience.
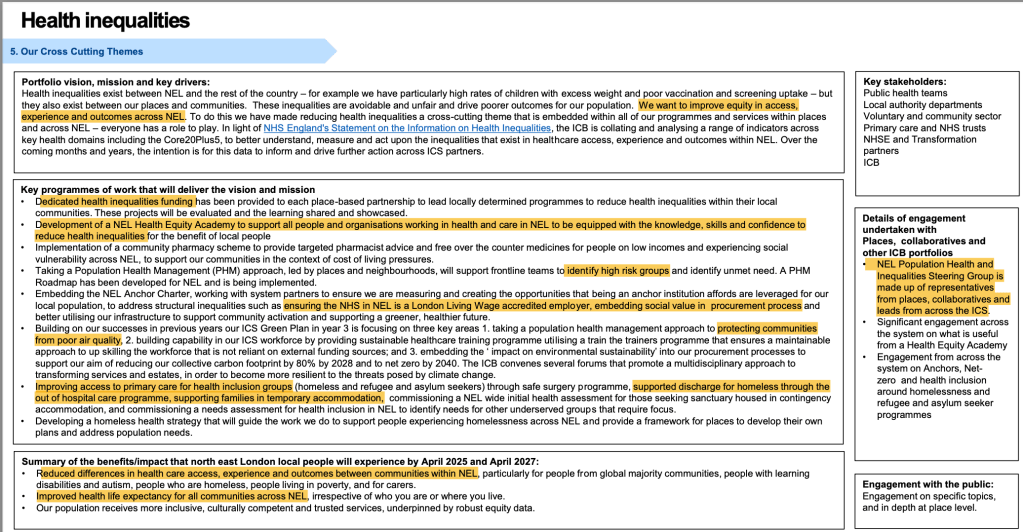
As I said in my earlier blog – I have prostate cancer. Unfortunately for me its a rare and rather nasty kind – Ductal Adenocarcinoma. The little table below (via CHATGPT) illustrates this.
| Measure | Estimated UK Figure |
| Annual prostate cancer diagnoses (men) | ≈ 50,000–65,000 per year |
| Proportion of all male cancers | ≈ 25% (1 in 4 male cancers) |
| Proportion that are ductal adenocarcinoma (DAC) | ≈ 0.1%–0.8% of prostate cancers |
| Estimated DAC cases per year | ≈ 60–480 cases annually |
| Notes on DAC classification | Figures include uncertainty due to rarity and mixed acinar/ductal histology |
After radiotherapy what next?
I have now completed a set of 20 days Radiotherapy and frankly, have no idea whether or not this has made any impact on the cancer.
The Cancer Hospital who are caring for me have no staff who have treated someone with this form of cancer. They have told me that I will be monitored – quite how I am not sure. They have offered a baseline MRI and continued monitoring of my PSA. DAC has only got a fairly weak link to abnormal PSA. I remain on a testosterone blocker.
So, I thought I would get a second opinion!
My first step was to go to Prostate Cancer UK. They provide a telephone advice service staffed by specialist nurses. I had two questions:
First, what does good look like with regard to monitoring Ductal Adenoma post treatment.
The answer was – there is no evidence base with regard to DAC so we cannot give any advice re good practice.
Second, can they advise me of any hospitals in the UK who have expertise in this field.
The answer was – it is not our policy to recommend particular hospitals.
I am an assertive middle class, white, former academic. I worry that other patients who lack my confidence (arrogance!?) connections and experience will not be heard and worse may even just ‘disappear’. This issue is increasingly recognised nationally.
I suspect my experience is similar to those experienced by people with other rare cancers.
What PCUK should do.
- First, a twin track approach. For most people with Prostate Cancer an evidence based approach makes sense. For people with rare cancers PCUK needs to establish an experience based approach. This means meeting with relevant oncologists and pulling together experience based best practice and sharing this.
- Second, making sure that individuals with rare cancers are connected to key charities and to the NHS so that they are not lost and where appropriate are signposted to specialist oncologists who may be able to help.
Why does this happen?
Clearly the vast majority of prostate cancer cases have a certain uniformity, and therefore the evidence base is clearer. I also suspect that NHS hospitals are driven by performance targets that are driven by the majority – rare cancers have no effect on hitting the target or not!
A hopeful future?
While I continue to try to work out what to do; the Governments new Cancer Plan has been published (4th Feb 2026) this has a whole chapter focussing on rare cancers and identifies a range of actions that are consistent with what I am saying and go further. This will clearly take time to see through … a commodity that people in my situation have not got!
I think that it is very important that clinicians and stakeholder charities such as Prostate UK and Macmillan start to work with the spirit of this ambition.
As for me, my GP and I will probably use what knowledge we can scrape together (CHATGPT again!) and see if we can identify and then get a second opinion from a hospital in the UK which has some expertise in this field.
As for people who are not confident, lack IT skills, have little experience of influencing systems – I have no idea what will happen to them in the interim.
WHAT DO YOU THINK?
Some of you will know that I was diagnosed with a rather rare form of prostate cancer earlier this year – I have now completed 20 days of radiotherapy … I have no idea if it worked or not. This blog is not about poor me! I want to share one of the things I learnt during radiotherapy and the action I took – I want your responses to that!
Just before I press on I just want to say that in response to my diagnosis one of my sons is running the London Marathon next year raising money for Prostate Cancer Research – it would be great if you can support him – the link is here.
ANYWAY!
I had radiotherapy for prostate cancer and the treatment finished a month ago. During that time the following thought occurred to me.
There are three key players during radiotherapy for Prostate Cancer.
- The fantastic technicians who manage the process and make the machines work.
- The incredible machines that scan and irradiate us.
- Us men who are being irradiated.
I want to talk about the men.
The NHS rightly focusses on ensuring good clinical practice however it fails to recognise just how important patients are – both individually and collectively.
During my treatment for a period of time each day (about 40minutes to an hour) I was part of a group of men who together were waiting to be scanned and treated.
This was peer support – we were an informal support group.
We got to know each other, we chatted about our concerns and most importantly how we manage the FBEC rule. FBEC means Full Bladder Empty Colon that is the status we had to achieve before treatment each day.
The chat was usually dry, caring and a bit humorous. Before radiotherapy you are scanned to see if you have met the FBEC test. If you don’t you are sent out to rectify the situation – you have three goes – if you fail all of these then another day is added to your programme.
Prompted by this experience I produced a badge.
I wanted the badge to commemorate our experience, in a small way to raise the profile of this treatment and to flag up to other men who are also going through this process that they are not alone.
In a gentle way the idea is to flag that a group of men sitting together and chatting is actually an important part of the process.
I sent the badge with an Badge Letter to the 25 or so hospitals in the UK that provide radiotherapy. Suggesting they might want to make the badge freely available to men who are members of this club and also suggesting that very short leaflets written by patients about what they learnt could be included.
After three weeks I had three replies. One from Prostate Cancer UK and the other two from hospitals.
I suppose I should not have been surprised – but responses so far have included – and I paraphrase:
‘We already provide personalised communication about this issue for patients – one to one’ This is great of course – but rather misses the point that a group of adult men talking and sharing their experiences brings a different sort of value.
‘If we provide this badge to prostate cancer patients then everyone would want one’ I really don’t think this is a particularly strong argument!
What I learnt
I suppose I should not be surprised. Despite the excellent clinical expertise it feels that the role of patients as active partners in supporting each other is not really understood by many clinicians.
Of course it could just be that the badge idea is really naff!
What do you think?
Don’t Silence the Patient Voice: Why Abolishing Healthwatch is a Mistake
Abolishing local Healthwatch is NOT a foregone conclusion – now is the time for MPs and national and local allies to defend independent public voice in health and care
The NHS 10 year plan flags that the Government intends to abolish local Healthwatch. This is part of a wider move away from independent public voice – replacing it with individual NHS apps and a reliance on NHS providers and commissioners doing public involvement better.
You can read my initial critique of this proposal here.
In order to abolish local Healthwatch – an Act will need to be passed in Parliament.
This means that Local Healthwatch will continue to exist for at least another year – possibly two.
You can see a probable timeline here – notice that it is at least a year long.
We live in a democracy
Lobbying to change legislation is part of the democratic process.
It is the case that a number of local Healthwatch are talking to local leaders including MPs and local authorities to gather allies to seek to change this proposal and identify alternatives if the Act is passed unchanged.
Isn’t there good evidence that local Healthwatch should be abolished?
Actually the evidence base for this decision is very thin. Here is a summary of the rationale from the Penny Dash review for DHSC on patient safety (2025) and parallel rebuttals from me highlighting analytical weaknesses.
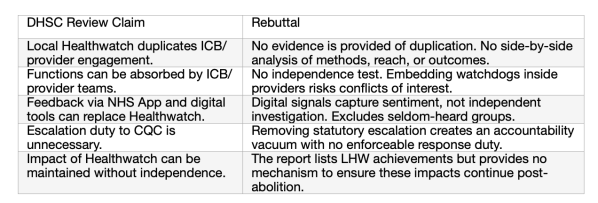
There is a bit more detail to download here.
The rationale for abolishing local Healthwatch is weak. Abolishing it weakens independence and public voice, reduces equity and removes statutory accountability mechanisms.
Who cares that local Healthwatch is being abolished?
There is an online petition organised by local Healthwatch here.
There is also a second early day motion launched by the Liberal Democrats here.
Many reputable organisations have expressed considerable concern about the abolition of local Healthwatch.
- The King’s Fund — Long read unpicks the plan and flags risks to independent patient voice; explicitly notes the plan would abolish Healthwatch England.
Nuffield Trust — Questions deliverability and capacity, warning that over‑centralisation and unclear accountability could undermine aims.
The Health Foundation — Analysis argues the plan’s policy mix lacks clarity and coherence, risking distraction from core improvement and equity. - NHS Confederation — Explains what’s in the plan and highlights practical risks during transition, including governance and oversight gaps.
National Voices — Umbrella body for charities warns against weakening patient and public involvement structures.
Patients Association — States closure would remove a vital, independent route for people to be heard and for services to learn.
BMJ (News) — Reports patient leaders’ concerns that replacing independent safety bodies and patient‑voice mechanisms could undermine safety.
More detail is available here.
There are so many expressions of concern out there – here a just a few:
Why is there no national campaign then?
This is probably because Healthwatch England has largely accepted that the proposals in the legislation will become law. In other words it is doing its best to close local Healthwatch in an orderly way.
It is interesting to see that the current Chief Executive of Healthwatch England is now a non Exec Director of NHS England. NHS England will of course NOT be publicly opposing any of the actions in the 10 year plan!
In fairness to Healthwatch England it is part of the Care Quality Commission and is therefore constrained with regard to lobbying in a way that independent local Healthwatch are not.
However a quick analysis of the Healthwatch England approach shows that while constrained by its legislative position it has also failed to utilise its strategic position.
Healthwatch England’s statutory design inside the CQC explains why it did not front a national campaign or petition: it lacks formal campaigning powers and is structurally dependent on the Department of Health and Social Care.
However, this does not explain the absence of strong, evidence-based interventions. HWE could have:
- Published authoritative independence and accountability analyses; • Highlighted statutory powers (Enter & View) that would be lost;
- Coordinated national media stories and external coalition support;
- Equipped MPs, Peers and the local Healthwatch network with amendment packs and briefings.
- In short, the weakness of HWE’s response is only partly due to its legal constraints. The greater issue is a lack of strategic leadership and failure to exploit the tools available within its remit. This has left the defence of independent Local Healthwatch largely to local bodies and external allies.
- There is more detail in this short briefing here
The abolition of local Healthwatch is not a forgone conclusion. In my view it is very unfortunate that Healthwatch England has accepted the 10 year plan proposal and is currently talking to key players such as the Local Government Association and DCLG about the wind down of local Healthwatch rather than about how they can be defended.
As citizens and independent organisations we have the right to lobby government and to challenge proposed legislative change.
Now is not the time to be scurrying around trying to tidy everything up with local government (the commissioners) this should be after/if the legislation has been passed.
There is still plenty of time to call for a rethink.
It is clear that Healthwatch England does not represent the views of local Healthwatch who are independent local organisations. Many are are pursuing a course of action that is different to that of Healthwatch England.
This is more than the survival of local Healthwatch – this is about arguing for a local based, independent voice which supports local people collectively to raise concerns about their health and care services.
WHAT DO YOU THINK?
At the centre of the government’s Fit for the Future (FFF)is a loss of heart – replaced by an inward looking managerialist response to complex challenges. The NHS is ours. We need governments to enable citizens to engage with services, to work alongside, to actively discuss and challenge.
The plan recognises the importance of addressing quality and pays lip service to the primacy of place. Yet it fails to understand what actions are needed to drive improvement and empower services to improve.
The FFF rightly highlights the litany of terrible high profile failures such as Mid Staffordshire, East Kent Hospitals, etc (p86).
It goes on to say that it is essential to put patient choice, voice and feedback at the heart of how we define and measure quality.
Yet … it shows no understanding of the important role played by organised collectives of the public to get many of these issues heard. From Grenfell through to Windrush, Infected Blood Scandal etc. The people who were affected and their supporters came together to campaign, whistleblow and challenge. These campaigns should not have been needed – but were an important and necessary contribution to highlighting serious deficits in the system.
The reality is that complex democratic systems will always require external challenge led by the public. There is a delusion that the solution is only about being better managers … over a system where we will never be in complete control, we need to celebrate this public challenge and make it easier for it to happen.
Local places need to be able to provide a locus for this external, public led challenge.
This is why it is so foolish to propose getting rid of Local Healthwatch.
The 10 Year Plan instead focusses on the primacy of individual experience over collective action.
- We see a slashing of any intervention that brings the independent voice of the public to challenge the NHS from the outside – such as local Healthwatch. At their best local Healthwatch are important partners to functions such as the Local Health Overview and Scrutiny Committee and through their actions they have empowered NHS staff who lack the confidence to speak up on issues they know need addressing.
- There is an incorrect and naive assumption that ‘moving this tiny function inside the NHS will somehow retain it. (P89) Get real – taking a couple of staff who work in a specialist organisation focussed on public challenge and putting them in an organisation where this activity is marginal to their day to day – will not work. For goodness sake (as FFF notes) they have enough difficulty accommodating internal whistle blowers!
- Separation of the residual local Healthwatch resource into local government social care and the NHS ICB which fails to recognise just how integrated these services are in terms of many peoples experience (eg older, people with disabilities etc)
- A weakening of the public voice on Foundation Trusts – saying that it is not compulsory for NHS Trusts to have public governors anymore – p81
- The proposal to trial “Patient Power Payments” (p83), feels like more soundbite nonsense. A belief that improvement can be driven through allowing patients to decide if they are happy with a service by having the power to determine whether or not the final cost of a service can be paid over to the relevant provider. How is this going to work exactly? Patients paying over the ‘tip’ for surgery? GP appointments? A prescription letter? The effectiveness of Statins? The chat with the GP? Who will do the admin?
- The reliance on the holy grail of a single NHS App – one app to rule them all! Which will allow patients to refer themselves for some treatments, choose providers, leave feedback. There is no recognition of the digital deficits faced by many people which will widen the inequalities gap.
- There is no humility – how about learning from (and collaborating with?) exemplary independent providers such as Care Opinion who magically bring together qualitative and quantitative public experience of social and health care services and engage providers in these stories.
At the core of FFF is a loss of heart – replaced by poor quality analysis which does not appear to know what drives change. The NHS is ours. We need governments to enable citizens to engage with services, to work alongside, to actively discuss and challenge.
Instead we see poor quality technocratic solutions put forward which individualise peoples experiences and a massacre of independent public voice organisations which could help us to come together, share our experiences and our ideas and contribute to positive change.
What do you think?
For some of the background to this see – my blog on Healthwatch England from last year
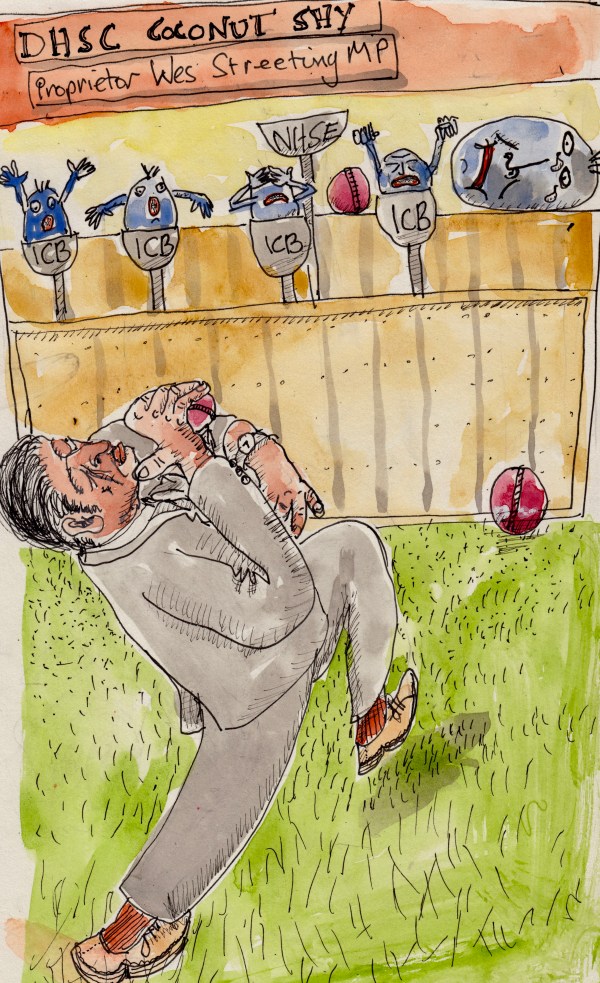
The above quote is from page 89 of Fit for the Future – 10 year health plan for England it gives an insight into the quality of analysis held by the writers of this report.
From a quick web search I think for the year 2023 the number of complaints referred to the health and rail service ombudsman were as follows:
On the surface the assertion in the quote is about right.
However, these are tiny figures. There are something like 600m patient contacts in the NHS in England every year, and about 1.6bn passenger journeys on the railways in the UK.
You can only be referred to the Ombudsman if you have already complained to the organisation concerned and it could not solve your problem. I suspect because train complaints are simpler a greater proportion will be resolved by the company concerned.
Although about 3 times more people use rail every year compared to using the NHS we are not comparing like with like here.
- Compared to the NHS rail has relatively few organisations involved – roughly 30 compared to approximately 4,000 NHS organisations including trusts, ambulance services, dentists etc etc.
- These figures show the number of referred complaints – they are not an indication of the number of complaints that were accepted as valid by the Ombudsman or the number of complaints received and resolved by the receiving provider.
- Thank goodness people complain about their NHS. Our health is central to who we are. Complaints will include those from people who are upset and frightened. This is a completely different order to peoples experience of trains. We probably want more complaints rather than fewer ones.
- The human body and its ailments are a bit more complicated than trains. We built trains, we know how they work. We didn’t build people – any clinician worth their salt will tell you that we do not know everything about illness and its cures. Yet, many of us who use services look to clinicians to have definitive answers – this is often not possible.
To conclude
You may say – ‘why is he worried about 20 or so words in a 169 page report?’
This soundbite phrase in a serious report is an indication of the poor quality of the thinking and analysis of the people who wrote this document and regrettably follows through to other more serious proposals in the document as a whole. Which I will try to comment on soon.
I think this specious soundbite is there to justify some of the proposals in the report by painting a picture of organisational incompetence in the NHS.
That is shameful.
What do you think?
One of the reasons why the NHS bodies with the longest history – hospitals – know that they only need to respond VERRRY slowly to NHS commissioners is because the next time they look those commissioners will be gone and replaced by another structure.
Here we go again
The government is:
- Abolishing the arms length body NHS England – subsuming some of its functions into the Department of Health and Social Care.
- Cutting the management budgets of the sub-regional Integrated Care Boards in half.
Some thoughts.
I have struggled to see the added value of NHSE. Many of its functions appear to have been either performance managing local NHS providers on behalf of the Government or allocating funds to local providers …. on behalf of government.
Generally speaking it appears to have struggled to bring a more independent voice that brings added value to Government Policy.
Having said this I think DHSC have benefitted from having NHSE because government has been able to say that it is NHSE who are responsible for allowing waiting times to grow and hospitals to over overspend. In theory this abolition will bring this accountability closer to Westminster. Unless there is someone else to blame of course.
Inequality
One of the areas that I am particularly worried about is health inequalities. I do think that Bola Owalabi’s team in NHSE has made significant strides in championing and embedding action on health inequalities in the wider NHS
I have concerns that the team will struggle if it is transferred into a Government department. My worry is that it will be at the mercy of a ministers in a way that was not the case at NHSE.
I cannot think where else this important function can go – the NHS Confederation maybe, the best option is possibly to be based with a ‘super ICB’ – see below.
Integrated Care Boards
As I flagged at the top Integrated Care Boards have until the end of 2025 to make cuts of 50% in their management costs. This is a real worry.
- They are still very young organisations and frankly most members of the public and many local decision makers have no idea that they exist or know what they do. From some work that I did for the NHS Confederation I think that there are a number who have made a significant impact (for example West Yorkshire, North East London) these have a sophisticated understanding of their local health and care system and a plan to change them for the better. Alas, there are almost certainly more who have taken a safer and less impactful approach.
- There is a distinction between ICB staff who are part of place teams (in South Yorkshire we have 4 place teams one each for Sheffield, Barnsley, Rotherham and Doncaster) and those staff who have a more corporate role. In my experience the place teams are crucial when it comes to influencing local providers about how they respond to population health challenges and utilise NHS funding. The most attractive model for me would be to merge ICB – so in Yorkshire and Humber have one not three. This would then permit place teams to be protected and (very) senior management to be reduced.
- One of the biggest problems that the NHS has been wrestling with for years is how to change the role of hospitals – in particular getting them to take more responsibility for population health. There are examples such as Kings and Guys & St Thomas Foundation who have made real strides here. These changes could be used to increase the accountability that Hospitals have to Government and could lay the foundation for a wider population health approach led by Hospitals in partnership with primary care, local government and the VCS. A small but important example of this is the Pathways work which was initiated by University College Hospital. Under the leadership of Aidan Halligan they took action on issues outside the hospital – homelessness because it affected their services.
I am not holding my breath.
There are interesting points of view here:
BMJ by David Oliver: Abolishing NHS England is no panacea for the NHS’s woes
and here: Andrew Harrison: Are ICB cuts a bigger story than NHS England?
What do you think?
At last! – Health and the role of neighbourhoods!

It is unusual for me to read a policy document from NHS England that I feel generally pretty positive about.
The launch at the end of January the NHSE Neighbourhood Health Guidelines might be an important and hopeful moment. However, in order for these guidelines to make a difference they must be used by local change agents in the statutory and voluntary sector as a platform to engage with, motivate and challenge NHS structures to respond and put in place actions that will fundamentally change current working practice.
Summary
These guidelines are the precursor to the publication of the next 10 year Health Plan.
They emphasise that the direction of travel is towards neighbourhood health and focus on 3 areas for action:
- Hospital to Community
- Treatment to Prevention
- Analogue to Digital
For 2026/6 the focus is on preventing people spending unnecessary time in hospital and care homes. This includes reinforcing links with wider public services, the third sector and local communities to fully transform the delivery of health and social care according to local needs.
The wider context and the need for more integrated working is recognised for example page 5 of the guidelines states:

The guidelines call on NHSE regional teams to work with local government partners to agree locally specific impacts which they will seek to achieve in 25/6 – these to include:
- Improve timely access to general practice, urgent and emergency care
- Prevent long term and costly admissions to hospital
- Prevent avoidable long term admissions to residential and nursing care.
It is refreshing that the document has no mention of social prescribing!
Some thoughts
While there are great examples of Integrated Care Boards who have laid foundations for this agenda such as West Yorkshire and North East London – I think there are also a number who are off the pace. I do wonder if these guidelines flag up the beginning of the end for Integrated Care Boards given the need to push management resources to place and maybe put some of the resource into NHSE regional structures.
I think that we should expect to see an urgent refresh of management resources at place. These must have a much greater emphasis on relational and community development skills including a more sophisticated relationship with local government that strengthens local accountability and decision making.
At its core we should see an assertive shift of funding from hospitals to neighbourhoods and as part of this the VCSE such as community organisations and key players such as welfare rights providers.
This emphasis on neighbourhood and place also affirms the role of local authorities as key lynch pins in health and care systems, strengthening their responsibilities to commission key organisations such as local Healthwatch.
Actions to take?
As I flagged at the beginning I think it is key that local change agents ensure that these guidelines are used to created discussions at a place level which are about the actions and changes that the NHS needs to take to deliver on these.
In part they must be used to generate critical discussions – fundamentally they should be used to test whether Integrated Care Boards understand and act on the need for change that is required. Frankly, Integrated Care Partnerships should take a lead in ensuring these challenging discussions happen.
We should expect:
- Critical reviews of how fit for purpose the NHS is to deliver on these guidelines actions now and in the future – these need to be discussed publicly and developed in partnership with local government and the VCSE.
- These reviews should have at their core the voices of neighbourhood communities, primary care networks and the VCSE.
- The reviews should provide a foundation for place strategies that in the first iteration identify actions that will ensure that the workforce and local accountability are fit for purpose.
- Place based strategies need to have explicit budgets attached to them that link back to the guideline priorities.
What do you think?
Robbing Peter to Pay Paul – Government imposes national insurance hike on voluntary sector
 This blog is written in a personal capacity and does not represent the views of Citizens Advice Sheffield. Also – treat my maths with caution!
This blog is written in a personal capacity and does not represent the views of Citizens Advice Sheffield. Also – treat my maths with caution!
The government plans to increase Employers National Insurance Contribution from 13.8% to 15% from April 2025.
I think the Chancellor has failed to understand what this means to the voluntary and community sector. Particularly those parts of the VCS where the majority of their income comes from contracts and grants from the local or national state.
Citizens Advice Services are a good example here. The overwhelming majority of local Citizens Advice funding comes from the following sources:
- Local Government
- The NHS
- Government Contracts
I am a trustee of Citizens Advice Sheffield – we are one of the largest local citizens advice in the country – in 22/23 we helped over 24,000 people in Sheffield, we brought in some £13m to the city and helped people resolve £1.4m of personal debt. We also helped thousands of people who were having problems with their energy supplier and provided a statutory advocacy service to over 2,000 people.
Impact of this increase
Currently our total income is approximately £6m – this includes a large contract to provide advocacy services in Sheffield.
Over 80% of our income is used to pay salaries. So in crude terms:
Current expenditure on salaries – £4.8m of which 13.8% is employers NI – so net expenditure on salaries is approximately £4.8m – £662400 = £4.1m
The impact of this National Insurance increase means that we will need to find roughly an additional £80,000 a year. This equates to 3 or so posts.
For years much of our income through contracts and grants has not received uplifts to keep in line with inflation – let alone this increase.
We face the following options:
- Reduce our establishment by 3 staff, which means will we help fewer people.
- Ask our funders to cover the costs – this means that local and national government organisations will in effect be putting tax revenue back into the treasury. Indeed some of it will be local government funding that will now go back to Westminster!
Lacks nuance.
Maybe the original thinking was that this is a tax on profit. It may work for companies who are making a large amount of profit and currently passing this on to shareholders etc.
The government appears to be treating some sections of the VCS as a special case such as Hospices. I am not going to criticise them at all – but it does feel as though the Government is being led by PR here – not by a strategic view of priorities.
It may even work with VCS organisations whose funding base is primarily charitable giving – for example the RNLI and Macmillan. In theory they can try to increase the amount of unrestricted funds by making further demands on the public for donations!
It is most iniquitous for VCSE organisations whose funding streams are predominantly based on contracts with the local and/or national state – there is no built in profit margin. Many of these contracts were won through competitive processes that emphasised low cost. Predictably, the contracts with the tightest margins are government contracts!
Impact
If organisations like Local Citizens Advice have to reduce the number of employees this has a number of effects.
- The government no longer gets the NI from the staff we did employ.
- We have fewer staff in our organisation – so we help fewer people. This means we put less money into the pockets of the most disadvantaged and we bring less money into Sheffield.
Westminster Debate
There has been a bit of a debate sponsored by Joe Robinson about the impact the NI increase will have on the voluntary sector. You can read this here. Not surprisingly most participation came from the conservative (whose policies meant that the VCS is already in poor shape) and liberal democratic opposition, although I was pleased to see that a couple of Lab0ur MPs including one of our Sheffield MPs (Abtisam Mohamed) raised concerns about this issue too.
What do you think?
What is the point of the NHS Integrated Care Board Plan?
This is about health inequality
When we at Leeds Beckett University interviewed Integrated Care Board(ICB) health inequalities leads as part of our work for the NHS Confederation one of the issues raised by an interviewee concerned Joint Forward Plans(JFP). These are produced every year, they set out what a particular ICB thinks the issues are and what actions they intend to take in response to these.
This health inequalities lead said:
“The joint forward plan is basically an NHS GCSE examination where there is a set of questions and there is a model answer and the model answer is the cultural norm that NHS England require. It doesn’t materially really affect the way the organisation behaves. It’s a necessary process that doesn’t add an awful lot of strategic value.”
Why read the JFP?
In my view the primary audience of a JFP should be local stakeholders not NHSE. Such stakeholders could be the manager of a local charity for example a Citizens Advice Bureau or a community anchor … or the clinical director for a primary care network.
They will want to know what the Integrated Care Board is doing about health inequalities and should feel it is worth reading the JFP to understand what NHS commissioners are planning to do and how this is relevant to their work.
For the JFP to be relevant it needs to be:
Easy to navigate
You don’t want to have to read a lengthy document to try to find the bit that is relevant to you!
Clear about analysis and actions
The JFP must make it easy to see how the ICB priorities link to those of local stakeholders, for example:
- How do they describe the health inequalities challenge?
- What actions are they proposing to take to tackle these?
- Who is responsible for these actions and how can they be influenced?
Most fundamentally how does this JFP help the reader to be better at tackling health inequalities in their role and how does it energise them and make them feel that the ICB is a potential collaborator?
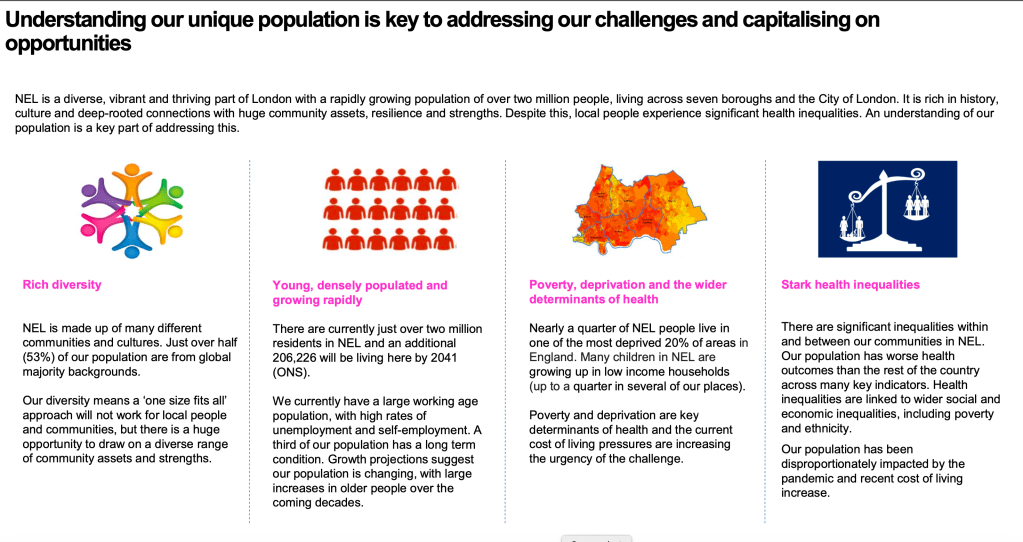
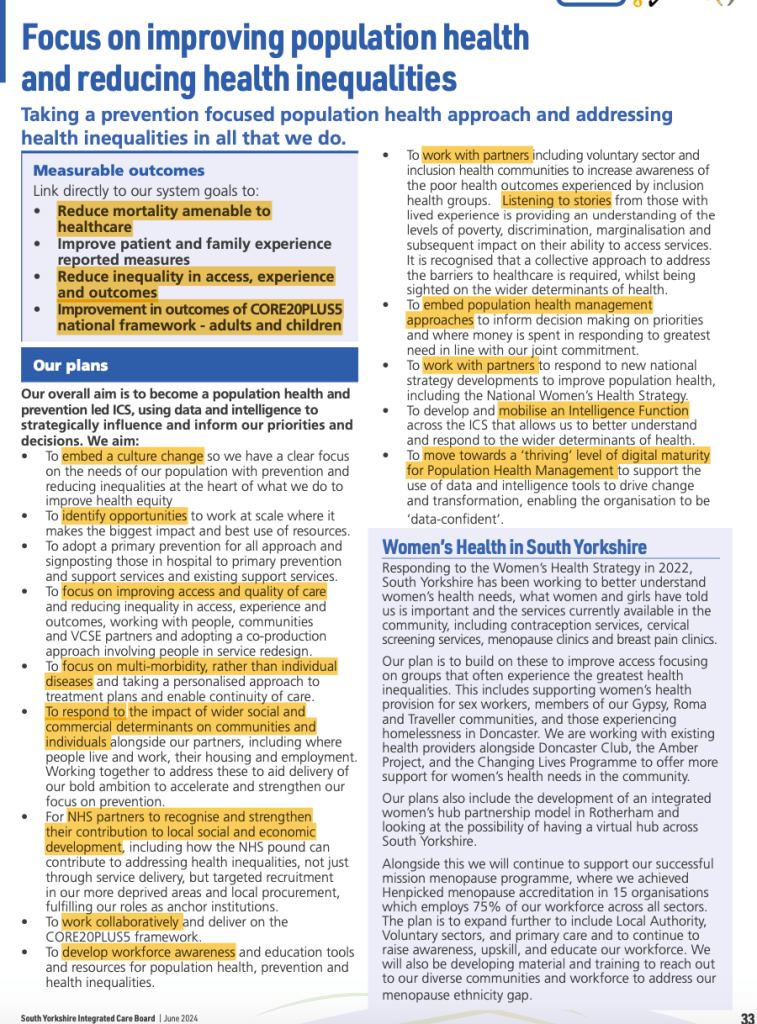
I have had a quick look at two 2024/5 JFPs – one from South Yorkshire (SY) and one from North East London (NEL).
Length matters
- The NEL JFP is 59 pages
- The SY JFP is 89 pages
Description of place
Both plans take about the same number of pages in their description of their population. I think NEL is more sophisticated. It uses design and crisp analysis to give a real feeling for who lives there, the nature of the area and makes an honest statement about inequality. It also starts to flag up priorities.
SY is ok but it struggles to make the leap from (fairly standard) data to – analysis to – priorities for action. We don’t get as much of a feel for the characteristics of the population and the presentation lacks energy.
Actions
Both JFP have a section on health inequalities. Screenshots of the relevant pages are below.
The NEL plan has a fairly explicit set of actions which are measurable. For example, allocating a specific amount of funding to each local authority area for health inequalities or supported discharge of the homeless.
The SY JFP is vague. Many of the ‘actions’ feel more like cultural ambitions and aren’t measurable. For example, embed a cultural change, focus on improving, work collaboratively etc. They fail to move from broad generic statements that sound good to specific actions. It is really not possible to understand what their priorities are and hence specific actions.
Who is responsible?
So, you’ve read the plan – you want to clarify something or maybe challenge or disagree; who do you talk to?
The NEL JFP – flags up what appears to be a pretty inclusive heath inequalities steering group … although there is no direct reference to it on their website or any information about agendas and minutes.
I have been told that South Yorkshire ICB has a similar albeit less representative group – however there is no mention of it in the JFP or on their website.
Have you read your JFP? What do you think? Leave a comment on the blog!
Finally – a little caveat – I try to keep my blogs to less than 700 words – so they inevitably provide only a limited description and analysis of the issue I am writing about!
What are Healthwatch England up to?
I am writing this blog in a personal capacity – these are my views.
I recently attended a working group convened by Healthwatch England (HWE) – that is developing actions that could lead to HWE making a case for taking over commissioning responsibilities for local Healthwatch from local authorities.
According to HWE this shift stems from discussions with local government, local healthwatch and a report they commissioned from the independent consultancy Kaleidoscope – unfortunately this report does not appear to be publicly available.
This extract from the papers of the Healthwatch England Board held in May 2024 states:
My reading of the Kaleidoscope report does not make me think that their primary recommendation was to transfer commissioning responsibilities. This was one of the options they put forward. From conversations I have had with local government colleagues and with some local Healthwatch there does not seem to be a desire for commissioning to be transferred to HWE – I accept that there may be some local Healthwatch who have this view.
Why the transfer of commissioning?
The rationale for this seems to stem from concerns that we are all familiar with:
- Variation in the quality of local Healthwatch
- Variation in the level of funding for local Healthwatch
- Cuts in funding to local Healthwatch
- Conflict of interest between local authority commissioners and local Healthwatch
- The complexity of the Patient and Public Voice system
I have no problem with any of the above issues – they all exist. Indeed they exist in other organisations which are commissioned nationally such as the NHS! However, variation is not always negative – there are positives too. There are excellent local Healthwatch and many local authorities have done their best to support and protect local Healthwatch in the teeth of vicious central government cuts to local government.
With regard to conflict of interest – moving commissioning of local Healthwatch to a single rather weak national organisation which is very close to government appears to carry the potential for even greater conflict of interest?
Problems
Experience – HWE has no experience of commissioning at all. The idea that they can somehow pick up on this complex agenda, managing contracts, performance management etc feels naive and reckless. Many local authorities are actually rather good at this!
Money – local authorities bear the cost of commissioning local Healthwatch – if HWE were to take up commissioning funding for this would have to be found from somewhere?
Politics – this is really not the time to be crying “wolf” about local Healthwatch performance and local government performance with a new government just getting its head around functions and looking to save money! There are many examples of positive commissioning and good practice which should be built on rather than dismantling the whole system and resetting with an organisation with no track record of commissioning.
ICB/S – floating around in these proposals is a notion that commissioning can be done more cost effectively and efficiently at Integrated Care System level. If this is real, it completely misses the point about the democratic role of local government and place. Again, many local authorities and local Healthwatch are actually rather good at working with the complicated relationships in a place – they are part of it!
NHS – Its as sure as eggs is eggs that government will reorganise the NHS commissioning structures and ICS will change or disappear. This is not the foundation to build on – it is local authorities that are permanent and responsible for local democratic systems.
Focus should be on Healthwatch England
While it is tempting to think that the problems that exist can be solved simply by changing who commissions – this is wrong.
I think more can be gained by reviewing how HWE works. What has not worked? Where it should be focus? For example learning from the LGA Peer Challenge and the NHS Confederation Member Forums and developing much better knowledge exchange between peers.
Further, I think that HWE should be putting more energy into developing a systematic plan to influencing NHS and DHSC strategy development to ensure that the pivotal role that local Healthwatch can play is clear and mandated in all local health and care systems. Greater recognition of the potential role that local Healthwatch can play would help to address the confusing array of Patient/Public Voice activities locally.
What do you think?